Introduction
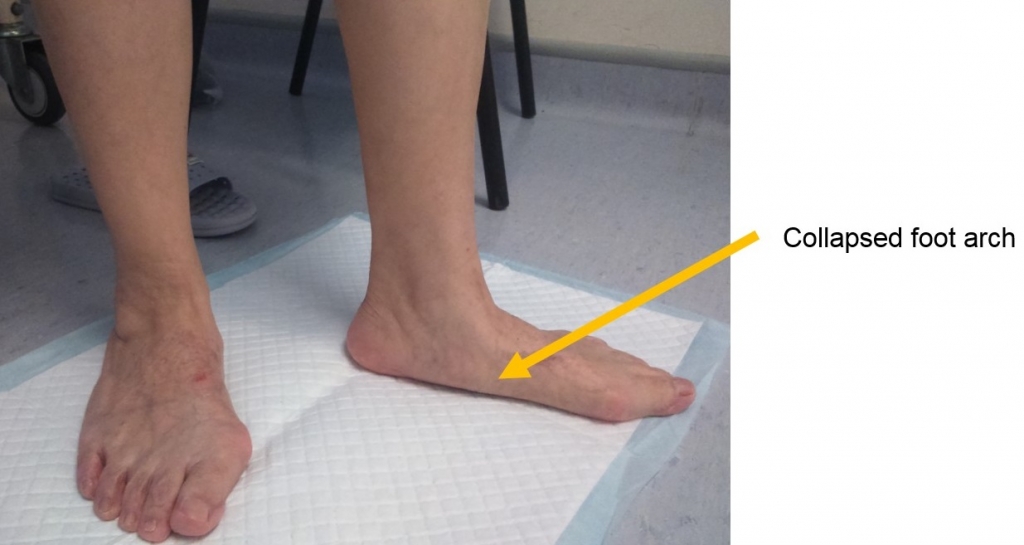
Adult acquired flatfoot deformity (AAFD) is also known as posterior tibial tendon (PTT) dysfunction or insufficiency. More recently, some literature described it as progressive collapsing foot deformity (PCFD). They all refer to the same problem related to the posterior tibial tendon which is a primary dynamic support to the longitudinal foot arch. [Figure 1]

AAFD is more common in women. The exact etiology is unknown. In the early stage, inflammation of posterior tibial tendon can lead to loss of foot arch. In the later stage, there could be degenerative changes in the midfoot joints.
Risk Factors
Patients who are at risk:
- Overweight
- Hypertensive
- Diabetic
- History of inflammatory disease
- Use of corticosteroids
- Pre-existing flat foot deformity
Symptoms
Patients may present with foot pain and weakness. As time goes by, there could be progressive loss of foot arch. There could also be lateral ankle pain due to subfibular impingement. Patients are unable to perform tiptoe standing on one single leg.
Signs
Possible signs include:
- Pes planus deformity with forefoot in abduction, collapse of the longitudinal foot arch and hindfoot valgus deformity. [Figure 2, 3]
- In the later stage, tenderness along the subtalar joint, calcaneo-cuneiform joint and talo-navicular joint.
- Achilles tendon tightness
- Intolerance in single leg standing
- Diminished power of the posterior tibial tendon
- Rigid deformities in which the foot could not be corrected to plantigrade position
Diagnosis
Standing radiographs could be done to evaluate the condition. Magnetic Resonance Imaging (MRI) is recommended to assess the severity of tendon degeneration and associated midfoot joint degenerations.
Staging
There are four stages based on severity of the deformity:
Stage I presents with flatfoot without deformity. Inflammation of the posterior tibial tendon may be present.
Stage II is a deformity which is still correctable passively.
Stage III is a fixed deformity with degenerative changes over midfoot joints. [Figure 4]
Stage IV involves deformity of the ankle besides the foot.

Treatment
Conservative treatments
- Anti-inflammatory drugs – Medications including non-steroidal anti-inflammatory drugs (NSAIDs) can be used.
- Molded insoles – They are useful in early disease to provide some pain relief and support to the foot arch. Nowadays with the improvement of technology, custom-made orthoses are readily available with 3D printing techniques to allow better fitting and quality of the insoles.
- Immobilization – Sometimes casting or walker is required to provide a better environment for the posterior tibial tendon to heal.
- Physiotherapy – Following a period of immobilization, physiotherapy could be started to stretch the Achilles tendon, strengthen the muscles and improve proprioception.
Surgical treatments
If conservative treatments fail, surgery can be considered. In the early stage, surgery consists of soft tissue reconstruction, tendon transfer and correction of alignment by osteotomies. In the later stage, fusion of the degenerative joints might be a better option. [Figure 5-6]


References
- Bubra PS, Keighley G, Rateesh S et al. Posterior tibial tendon dysfunction: an overlooked cause of foot deformity. J Family Med Prim Care. 2015; 4(1):26-29.
- Deland JT. Adult-acquired flatfoot deformity. J Am Acad Orthop Surg. 2008; 16: 399–406.
- Zaw H, Calder JD. Operative management options for symptomatic flexible adult acquired flatfoot deformity: A review. Knee Surg Sports Traumatol Arthrosc. 2010;18:135–42.
- Johnson KA, Strom DE: Tibialis posterior tendon dysfunction. Clin Orthop Relat Res 1989;239:196-206.
- Myerson MS: Adult acquired flatfoot deformity: Treatment of dysfunction of the posterior tibial tendon. Instr Course Lect 1997;46:393-405.
Written by Dr. Diane Tai Hei-yan
March 2021