Introduction
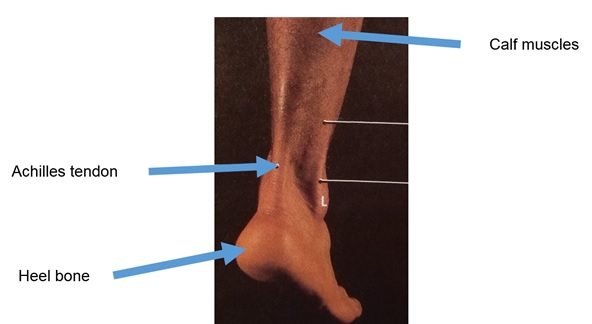
Achilles tendon is a thick band of fibrous tissue connecting the calf muscles (gastrocnemius and soleus) to the calcaneus (heel bone). [Figure 1] It is the largest tendon in our body. In front of Achilles tendon is the retrocalcaneal bursa which is cushioned between Achilles tendon and the calcaneus.
Terminology
Para-tendonitis is the inflammation of the tendon sheath where fluid accumulates around the tendon. However, Achilles tendon itself is not inflamed.
Achilles tendinitis is the acute inflammation of Achilles tendon.
Achilles tendinosis is the chronic degeneration of Achilles tendon. It might be secondary to para-tendonitis which leads to decreased blood flow to Achilles tendon. More importantly, Achilles tendinosis may be a predisposing factor to Achilles tendon rupture.
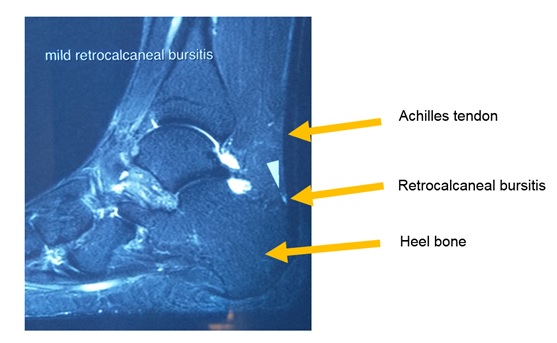
Retrocalcaneal bursitis is used to describe when the retrocalcaneal bursa is also inflamed. [Figure 2]
Achilles tendinopathy is used to describe an Achilles tendon pathology where there is a combination of pain, swelling and impaired performance. It could be acute or chronic. It could be classified according to its anatomical locations. If the pathology is near the insertion of Achilles tendon to the heel bone, it is called insertional tendinopathy. If the pathology is 2 to 6 cm above the heel bone, it is called non-insertional tendinopathy.
Risk Factors
Over-pronated foot or incorrect footwear can lead to Achilles tendonitis. Running downhill, exercise without proper warm-up, calf muscles straining after repeated exercise, and playing sports which require sudden stop, e.g. tennis, are also risk factors. People with tight heel cord are more likely to develop Achilles tendonitis as well.
Symptoms
Patients with Achilles tendonitis may experience pain after immobility e.g. walking in the morning. The pain can exacerbate during activities at day time. It could be sharp in nature. There might also be pain on single leg stand. This pain could be ongoing or recurrent over the Achilles tendon and become chronic Achilles tendinosis.
Signs
There could be local tenderness along the Achilles tendon. Calf atrophy, swelling and thickening could develop in chronic cases.
Investigation
MRI or ultrasound ankle could be performed to assess the extent of degeneration and degree of tendonitis.
Treatment
Conservative treatment
- Rest and activity modification – In the phase of acute inflammation, try to avoid high impact activities that will stress your Achilles tendon, such as running. If you would like to do exercises, please take it slowly and do adequate warm-up exercises beforehand.
- Ice therapy and anti-inflammatory drugs – Place the ice bag over the most affected area of the heel for at most 20 minutes or until the area is numb. Non-steroidal anti-inflammatory drugs such as Ibuprofen can be used to reduce pain and swelling.
- Orthosis – Heel pads are sometimes used to reduce stress to Achilles tendon. It could help relieve tension on Achilles tendon and reduce irritations from the back of shoe.
- Ultrasound and shock wave therapy – Ultrasound therapy is often administered by physio therapist to reduce swelling and inflammation. The high energy shock wave impulses could aid healing of the damaged Achilles tendon tissue in chronic Achilles tendinosis. However, it is not indicated in acute cases.
- Further strengthening and exercises – After the acute phase, gentle stretching of calf muscles could be commenced. Heavy slow resistance (HSR) training program is usually recommended. Cycling and swimming are good sports to start with. Running should be resumed until symptoms resolve. It is advised to have proper footwear for running and avoid hill running to prevent recurrence.
- Steroid injections – These are not recommended as some research studies showed that it might weaken the tendon and predispose it to rupture.
- Platelet-rich plasma (PRP) injections – PRP is made from a small blood sample of your own, centrifuged to concentrate the platelets in that blood sample. [Figure 3] PRP is rich in growth factors which can speed up the normal healing process in the affected area. Newer evidence showed that PRP produce good overall results for the treatment of Achilles tendinopathy up to a medium-term follow-up.

Surgical treatment
Achilles tendonitis usually does not require surgery. If conservative treatments fail after 3 to 6 months, surgery could be considered for excision of degenerated tissue and calcific deposits. [Figure 4] If Achilles tendonitis is not treated properly, there is an increased risk of Achilles tendon rupture. In that case, surgical repair is required. [Figure 5-6]



References
- Grants Atlas of Anatomy. 9th Edition. Anne M.R. Agur. Williams & Wilkins.
- Maffulli N., Florio A., Osti L. et al. Achilles Tendinopathy, JBJS Reviews. 2014 Sep; 2 (9): e5.
- Li HY, Hua YH. Achilles Tendinopathy: Current Concepts about the Basic Science and Clinical Treatments. Biomed Res Int. 2016; 2016: 6492597.
- Maffulli N., Khan K. M., Puddu G. Overuse tendon conditions: time to change a confusing terminology. Arthroscopy. 1998; 14(8):840–843.
- Van Dijk CN, van Sterkenburg MN, Wiegerinck JI et al. Terminology for Achilles tendon related disorders. Knee Surg Sports Traumatol Arthrosc. 2011 May; 19(5):835-41.
- Alfredson H, Cook J. A treatment algorithm for managing Achilles tendinopathy: new treatment options. Br J Sports Med. 2007; 41(4):211-216.
- Filardo G, Kon E, Di Matteo B et al. Platelet-rich plasma injections for the treatment of refractory Achilles tendinopathy: results at 4 years. Blood Transfus. 2014 Oct; 12(4):533-40.
Written by Dr. Diane Tai Hei-yan
25 January 2021
