Introduction
Ankle sprain is an injury to the ligaments which stabilize the ankle. In acute injury, most of the time it resolves with conservative treatment. It could be mild which requires no more than rest, ice therapy, compression and elevation. It could also be severe that the ligaments could be partially or completely torn depending on the severity of injury. With proper treatments, recurrent ankle sprain could be prevented. Otherwise it could lead to long term complications including recurrent instability symptoms, ankle arthritis and chronic pain.
Anatomy
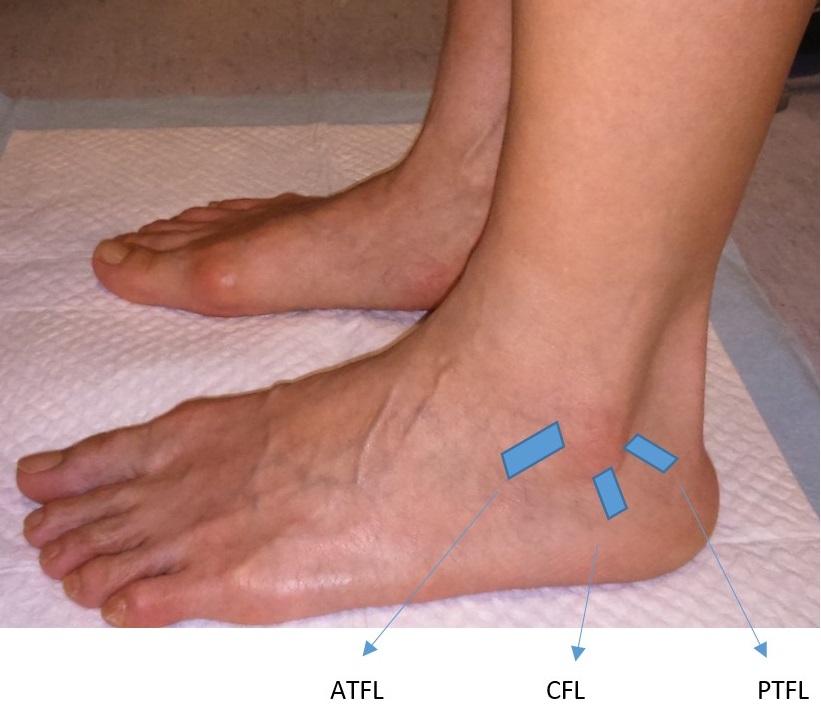
Ligaments are strong fibrous tissues that connect bones. Ankle sprain involves injury to the ligaments frequently on the outside of ankle. Patients are typically injured with a twisted foot and ankle. The ligaments on the inner side of ankle could also be injured but less commonly. There are three ligaments on the outside of ankle, namely anterior talofibular ligament (ATFL), calcaneofibular ligament (CFL) and posterior talofibular ligament (PTFL) [Figure 1]. Among these three ligaments, ATFL is the weakest and the commonest ligament to be injured among the above three.
Risk Factors
You may twist your foot and ankle during walking or running especially on uneven surfaces. There are some other risk factors including general ligamentous laxity, decreased proprioception, improper footwear, inadequate warm-up exercise and playing indoor court sports such as basketball and volleyball.
Symptoms
Patients complain of ankle pain, bruises and swelling after acute injuries. There could be difficulty in weight bearing walking. Recurrent sprain could follow in the long run if not properly treated. Instability is the terminology used to describe the sense of being unstable in holding the ankle in place on weight bearing, during strenuous activities or walking on uneven surfaces. Acute injuries could lead to chronic ankle instability symptoms.
Signs
Patient might have generalized ligamentous laxity, high foot arch deformity and abnormal proprioception. There might be hindfoot varus malalignment, which means the heels are turned inside. There could also be local tenderness over the outside of ankle. Specific tests are used for testing the integrity of ankle ligaments. Positive tests indicate that the ligaments are lax and could not provide sufficient stability for the ankle. There are some associated injuries which needed to be ruled out during physical examination and investigation, including cartilage (which is the layer covering bones for smooth gliding of a joint) injury, tendon injury and bone fracture.
Investigations
X-ray are taken to rule out associated injuries as mentioned above. Stress views could be taken in chronic setting as it could be hurting during acute injuries. Ultrasound and Magnetic Resonance Imaging could be taken to assess if the ligaments are attenuated or torn.
Treatment
Treatment depends on the severity of sprain. For first-degree sprain, which means the ligaments are sprained but not torn, there is usually minor swelling. Simple measures include rest, ice therapy, compression therapy and elevation are sufficient. Patients usually recover quickly after one week without the need for bracing or protective weight bearing.
For second-degree sprain, some ligaments are partially torn. Walking could be difficult. Besides the measures recommended for first-degree sprain, bracing might be useful to help the ankle rest and heal, usually for about two weeks. Then physiotherapy is referred for the following specific treatments:
- Range of motion – Your physical therapist will provide some exercises for you to improve the range of motion of your ankle. At the beginning, your ankle may be stiff due to a period of immobilization with bracing. You need to start moving your ankle. This is very important to prevent stiffness.
- Proprioceptive training – Good balancing is paramount to prevent future sprain. Your physical therapist may add some training exercise for you to improve your balancing. One example is to throw and catch a ball with single-leg standing on your affected side. Another example is standing on a wobble ball.
- Strengthening – When your ankle swelling and pain resolve, more exercises could be added to improve the strength of muscles around your ankle, especially for the group of muscles on the outside of ankle.
- Gradual resumption of sports – You may wish to resume your sports activities gradually. This may vary among patients. For second degree sprain, usually it takes 4-6 weeks after injury to resume your full sports activities.
For third-degree sprain, which means some ligaments are completely torn. There will be ankle instability, severe swelling and bruising. Bracing is suggested for three weeks. Rehabilitation is similar to second-degree sprain. However, it usually takes 8-10 weeks after injury to resume your full sports activities.
Surgical treatment is advised if there is persistent ankle instability. Options include repair and reconstruction. Patients need to have good tissue quality for repair. For patients who have poor tissue quality, chronic ankle instability, high foot arch and generalized ligaments, reconstruction should be considered. Typically, the ligaments are reconstructed with a tissue graft from other ligaments or tendons around the ankle, e.g. peroneal brevis tendon. After surgery, there is usually a period of immobilization with cast or protective boot. Rehabilitation needs time to restore stability and strengthen. It may take weeks to months.
References
- Al-Mohrej OA, Al-Kenani NS. Acute ankle sprain: Conservative or surgical approach? EFORT Open Rev. 2016;1:28–38
- Chan KW, Ding BC, Mroczek KJ. Acute and chronic lateral ankle instability in the athlete. Bull NYU Hosp Jt Dis. 2011;69:17–26.
- Odak S, Ahluwalia R, Shivarathre DG, Mahmood A, Blucher N, Hennessy M, et al. Arthroscopic evaluation of impingement and osteochondral lesions in chronic lateral ankle instability. Foot Ankle Int. 2015;36:1045–9.
- McCriskin BJ, Cameron KL, Orr JD, Waterman BR. Management and prevention of acute and chronic lateral ankle instability in athletic patient populations. World J Orthop. 2015;6:161–71.
- Van Rijn RM, van Os AG, Bernsen RM, Luijsterburg PA, Koes BW, Bierma-Zeinstra SM. What is the clinical course of acute ankle sprains? A systematic literature review. Am J Med. 2008;121:324–31.e6.
- Maffulli N, Ferran NA. Management of acute and chronic ankle instability. J Am Acad Orthop Surg. 2008;16:608–15.
- Kobayashi T, Gamada K. Lateral ankle sprain and chronic ankle instability: A critical review. Foot Ankle Spec. 2014;7:298–326.
Written by Dr. Diane Tai Hei-yan
March 2021
